Table of Contents
Hey there! Today, we’re diving into a topic that’s both critical and fascinating—molecular classification of breast cancer. By the end of this chat, you’ll have a solid grasp on the different molecular subtypes of breast cancer and feel confident tackling questions like the ones in our MedQuiz scenario. Ready? Let’s jump in!
What is Molecular Classification in Breast Cancer?
Breast cancer isn’t just a single disease—it’s actually a collection of diseases with different behaviors and responses to treatment. Molecular classification helps us categorize these cancers based on their genetic makeup, giving us a clearer idea of how aggressive they are and what treatments will work best. Think of it like getting to know the “personality” of the cancer. Is it calm and slow-growing, or is it aggressive and likely to cause trouble?
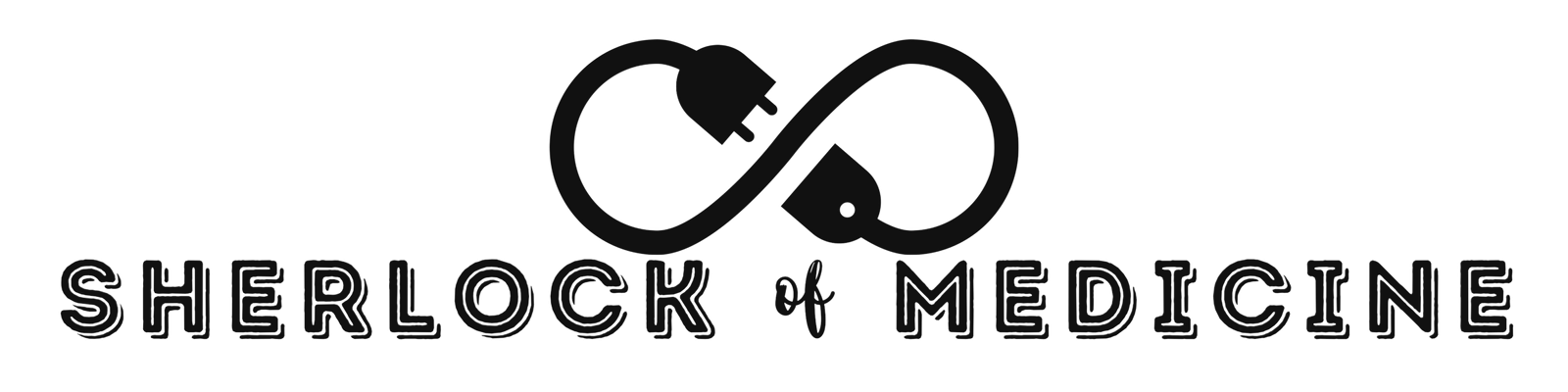
This classification process mainly relies on immunohistochemistry (IHC) tests, which look for specific receptors on the surface of the cancer cells. The big players here are:
– Estrogen Receptor (ER)
– Progesterone Receptor (PR)
– HER2/neu (Human Epidermal Growth Factor Receptor 2)
– Ki-67 (a marker of how fast the cells are dividing)
Let’s break down these components, one by one, to see how they guide us in understanding the cancer.
Hormone Receptor Status: ER and PR
First up, we’ve got ER and PR—the hormone receptors. These are like little antennas on the surface of some breast cancer cells that pick up signals from hormones like estrogen and progesterone.
– ER/PR Positive: If the cancer cells are ER or PR positive, they’re relying on these hormones to grow. These cancers tend to be slower-growing, and the good news is they often respond well to hormone therapy. Think of hormone therapy as a way to cut off the cancer’s fuel supply—it blocks or reduces the hormones, starving the cancer.
– ER/PR Negative: On the flip side, if the cancer is ER/PR negative, it doesn’t care about these hormones, so hormone therapy won’t be effective. This means we need to look at other treatment options.
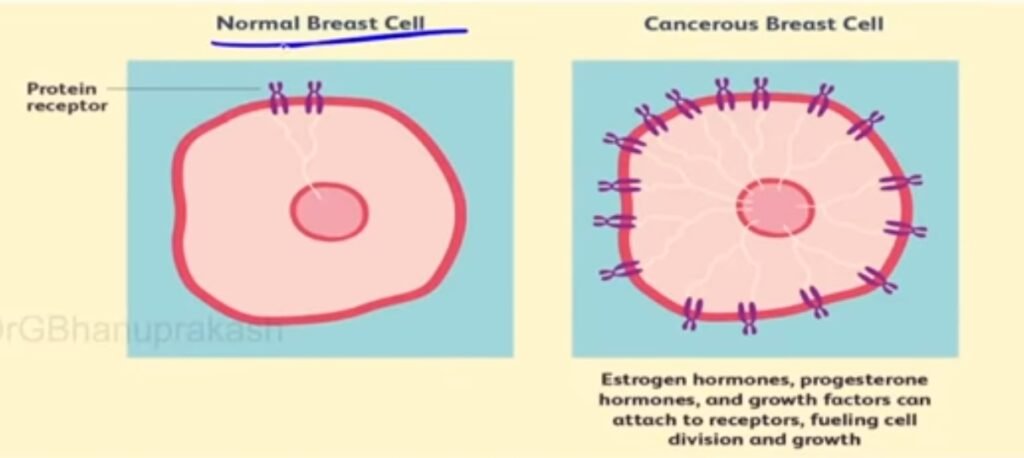
HER2/neu Status
Next, let’s talk about HER2/neu. This is another receptor, but instead of hormones, it’s all about growth signals.
– HER2 Positive: If a cancer is HER2 positive, it’s like the cells have their growth accelerator stuck in the “on” position—they grow and spread more aggressively. But don’t worry, we’ve got targeted therapies like trastuzumab (Herceptin) that can zero in on these HER2-positive cells and shut down their growth.
– HER2 Negative: If the cancer is HER2 negative, it doesn’t have this particular growth accelerator, so HER2-targeted therapies wouldn’t work. We’d need to consider other treatment strategies.
Ki-67 Index
Finally, there’s the Ki-67 index. This little number tells us how fast the cancer cells are dividing.
– Low Ki-67 (less than 15-20%): This suggests the cancer is taking its sweet time to grow, which is generally a good thing—it might mean a better prognosis and possibly less aggressive treatment.
– High Ki-67 (greater than 20%): If the Ki-67 is high, it means the cancer is growing quickly, and we might need to bring out the big guns with more aggressive treatments.
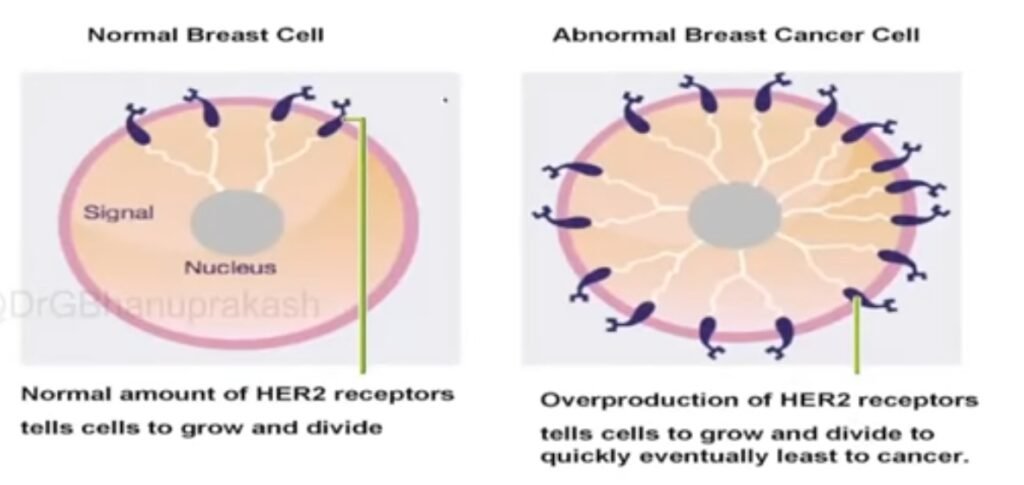
Putting It All Together: The Molecular Subtypes
Now, based on the ER, PR, HER2, and Ki-67 results, we can classify breast cancer into one of four major molecular subtypes. This is where the magic happens, as each subtype tells us something different about how to treat the cancer.
1.Luminal A
– ER/PR positive
– HER2 negative
– Low Ki-67
– Prognosis: Excellent. These cancers are like the chill, laid-back students who do well with just a little bit of guidance—in this case, hormone therapy.
- Luminal B
– ER/PR positive
– HER2 negative (or sometimes positive)
– High Ki-67
– Prognosis: These are the overachievers—they’re more active, so they might need a bit more attention, including possibly chemotherapy in addition to hormone therapy.
3.HER2-enriched
– ER/PR negative
– HER2 positive
– Prognosis: This subtype is a bit of a wild card—aggressive but responsive to targeted therapy like trastuzumab. It’s like having a fast car that you can control with the right tools.
4.Triple-negative
– ER/PR negative
– HER2 negative
– Prognosis: This is the tough one. Triple-negative cancers don’t have the typical receptors we can target, so they require a more aggressive approach, usually with chemotherapy
Applying This Knowledge: A Clinical Scenario
Now let’s revisit that clinical scenario we mentioned earlier:
A 52-year-old woman finds a lump in her breast, and the biopsy results come back like this:
– ER: Positive (80%)
– PR: Positive (60%)
– HER2: Negative
– Ki-67: 20%
What’s the molecular subtype?
Based on what we’ve learned, this profile fits the Luminal B subtype. It’s ER/PR positive, HER2 negative, with a high Ki-67 index. Remember, Luminal B cancers are more active, so they often require a combination of hormone therapy and chemotherapy to keep them in check.
Why It Is So Important?
Understanding the molecular subtype of breast cancer is crucial because it directly influences treatment decisions. For example:
Luminal A breast cancer is often treated with hormone therapy such as tamoxifen or aromatase inhibitors. These drugs block the cancer’s access to estrogen, which it needs to grow.
Luminal B cancers, being more aggressive, may require both hormone therapy and chemotherapy. Common chemotherapy agents include doxorubicin and cyclophosphamide, often followed by paclitaxel.
HER2-enriched breast cancer benefits from HER2-targeted therapies. Trastuzumab (Herceptin) is the most well-known, but others like pertuzumab (Perjeta) and ado-trastuzumab emtansine (Kadcyla) may also be used.
Triple-negative breast cancer, which lacks targeted therapy options, is usually treated with chemotherapy. Drugs like paclitaxel, docetaxel, or carboplatin are commonly used.
Knowing the molecular subtype helps us choose the right weapon in our arsenal, making treatment more effective and tailored to each patient’s unique cancer profile.
Practice
Now that you’ve got the basics down, it’s time to practice. Try applying this knowledge to different scenarios. Ask yourself:
– What would happen if the HER2 status were positive?
– How would a lower Ki-67 index change the treatment approach?
Remember, mastering molecular classification isn’t just about memorizing terms—it’s about understanding how these details translate into real-world, personalized care for each patient. The more you practice, the more confident you’ll become in making these critical decisions.
Final Thoughts
Whenever you need a refresher, come back to this blog. And don’t keep this knowledge to yourself—share it with your classmates, colleagues, or anyone who could benefit. The more we share, the better we all get at providing top-notch care. Keep practicing, stay curious, and remember—each question you answer brings you one step closer to becoming the skilled clinician you aspire to be.
Good luck with your MedQuiz, and remember, you’ve got this!
Related Articles

Understanding Molecular Classification of Breast Cancer In 5 minutes